Thyroid Cancer
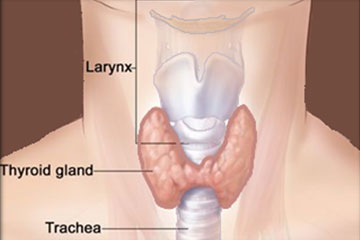
Thyroid Gland
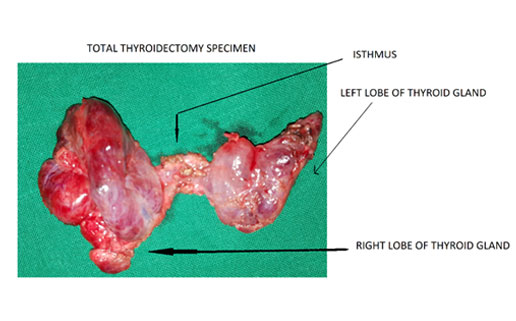
The thyroid is an endocrine gland in the neck consisting of two connected lobes (Right and Left on either side of the wind pipe, trachea). The lower two thirds of the lobes are connected by a thin band of tissue called the thyroid isthmus. The thyroid is located at the front of the neck, below the Adam's apple.
Thyroid Nodules -A lump in the thyroid is called a thyroid nodule.
Hypothyroidism-A condition in which the thyroid gland doesn't produce enough thyroid hormone.
Hyperthyroidism-The overproduction of thyroid hormone by thyroid gland.
Parathyroid glands are four small glands of the endocrine system which regulate the calcium in our bodies. Parathyroid glands are located in the neck behind the thyroid where they continuously monitor and regulate blood calcium levels.
THYROID CANCER
There are four main types of thyroid cancer. These are
1.Papillary Thyroid Cancer (Papillary is the most common type)
2.Follicular Thyroid Cancer
3.Medullary Thyroid Cancer
4.Anaplastic Thyroid Cancer.
Thyroid cancer is a disease in which malignant (cancer) cells form in the tissues of the thyroid gland. Thyroid cancer that is found at an early stage can often be treated successfully. Thyroid nodules are common but majority of them (80%) are not cancerous (Benign nodules). Extremes of age (Young below 15 and elderly above 50 years ), Females and persons exposed to radiation are at an increased risk of thyroid cancer. Medullary thyroid cancer is sometimes caused by a change in a gene that is passed from parent to child.
Presenting symptoms and Signs of Thyroid Cancer
Evaluation of a thyroid nodule
A thyroid nodule is an abnormal growth of thyroid cells in the thyroid. Nodules may be solid or fluid-filled. Following are the basic tests done for evaluation of any thyroid swelling or nodule –
- An Ultrasound of the Neck
- A (FNAC) fine-needle aspiration cytology. Usually an ultrasound guided FNAC is performed to get the sample exactly from the nodule under concern.
- Blood teststo check thyroid hormone levels (T3,T4 &TSH) and for antithyroid antibodies(ATA) in the blood.
- CT scan – For suspected cancer of thyroid gland, a contrast enhanced CT scan of neck may be advised for better evaluation of thyroid nodule and to confirm its spread within and outside the thyroid glands. CT scan is also more sensitive to detect spread of thyroid cancer to lymph nodes in the neck especially in the central compartment.
Thyroid cancer can also be classified as:
- Differentiated thyroid cancer- which includes well-differentiated tumours, poorly differentiated tumours, and undifferentiated tumours(Anaplastic); or
- Medullary thyroid cancer.
Well-differentiated tumours (papillary thyroid cancer and follicular thyroid cancer) can be treated and can usually be cured. Poorly differentiated and undifferentiated tumours (anaplastic thyroid cancer) are less common. These tumours are very aggressive and grow and spread quickly and have a poorer chance of recovery. Medullary thyroid cancer is a neuroendocrine tumour that develops in C cells of the thyroid. The C cells make a hormone (calcitonin) that helps maintain a healthy level of calcium in the blood.
Risk factors for thyroid cancer
These include the following:
- Age between 25 and 65 years old.
- Female gender.
- History of exposure to radiation to the head and neck as an infant or child or being exposed to radioactive fallout.
- Having a history of enlarged thyroid swelling (Goitre )
- Having a family history of thyroid disease or thyroid cancer.
- Having certain genetic conditions such as familial medullary thyroid cancer (FMTC), multiple endocrine neoplasia type 2A syndrome (MEN2A), or multiple endocrine neoplasia type 2B syndrome (MEN2B).
Medullary thyroid cancer
It is sometimes caused by a change in a gene that is passed from parent to child. The genes in cells carry hereditary information from parent to child. A certain change in the RET gene that is passed from parent to child (inherited) may cause medullary thyroid cancer. There is a genetic test that is used to check for the changed gene. The patient is tested first to see if he or she has the changed gene. If the patient has it, other family members may also be tested to find out if they are at increased risk for medullary thyroid cancer. Family members, including young children, who have the changed gene may have a thyroidectomy (surgery to remove the thyroid). This will decrease their chance of developing medullary thyroid cancer.
The Prognosis and treatment options depend on the following factors :
- Age
- The type of thyroid cancer.
- The stage of the thyroid cancer.
- Complete Removal in Surgery.
- General condition of patient.
- Genetic condition such as presence of multiple endocrine neoplasia type 2B (MEN 2B).
Stages of Thyroid Cancer
- Stages are used to describe thyroid cancer based on the type of thyroid cancer and the age of the patient:
- Papillary and follicular thyroid cancer in patients younger than 55 years
- Papillary and follicular thyroid cancer in patients 55 years and older
- Anaplastic thyroid cancer in patients of all ages
- Medullary thyroid cancer in patients of all ages
How does cancer spread in the body?
There are three different ways that cancer cell spread in the body.
Cancer can spread through local adjoining tissues, the lymph system, and the blood:
- Local Spread -The cancer spreads from where it began by growing into nearby areas.
- Lymphatic Spread -The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body. Papillary and medullary cancers have propensity to spread to regional lymph nodes in the neck. More than 50 % papillary and medullary cancers will have spread to regional lymph nodes in the neck at the time of diagnosis.
- Blood or Haematogenous Spread- The cancer spreads from where it began by getting into the blood vessels. The cancer cells then travel through the blood vessels to other parts of the body. Follicular Cancer of thyroid has high propensity to spread by haematogenous route to other parts of the body like liver and bones .
TREATMENT OF THYROID CANCER
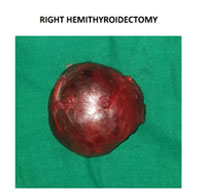
SURGICAL MANAGEMENT OF THYROID CANCER
Surgery is the most common treatment for thyroid cancer. One of the following procedures may be used:
Radiation therapy, including radioactive iodine therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or to arrest their growth. There are two types of radiation therapy:
Thyroid hormone therapy
Hormone therapy is a cancer treatment that removes hormones or blocks their action and stops cancer cells from growing. Hormones are substances made by glands in the body and circulated in the bloodstream. In the treatment of thyroid cancer, drugs may be given to prevent the body from making thyroid-stimulating hormone (TSH), a hormone that can increase the chance that thyroid cancer will grow or recur.
Also, because thyroid cancer treatment kills thyroid cells, the thyroid is not able to make enough thyroid hormone. Patients are given thyroid hormone replacement pills.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. There are different types of targeted therapy: