Oral Precancerous Lesions and Treatment
More than 500,000 new cases of head and neck squamous cell cancer arise annually worldwide, making it the sixth most common cancer. Of these oral cavity malignancies account for 14% and lead to upward of 7000 deaths per year.
Premalignant squamous lesions of the oral cavity are areas of altered epithelium that are at an increased risk for progression to squamous cell carcinoma (SCC). The most common of these lesions is leukoplakia and erythroplakia. About 50 % cancers do have such precancerous changes first before progressing to cancer. There is therefore a great potential in screening high risk individuals for such lesions and potentially prevent cancer. It is also a fact that up to 50% of oral SCCs cases arise from clinically normal mucosa.
Visible oral lesions such as leukoplakia, erythroplakia and erythroleukoplakia can alert health care providers to a premalignant disease process. Patients with these conditions experience a greater risk of developing oral cancer than the remainder of the population.
Leukoplakia
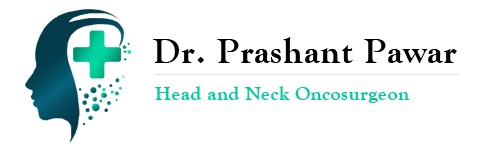
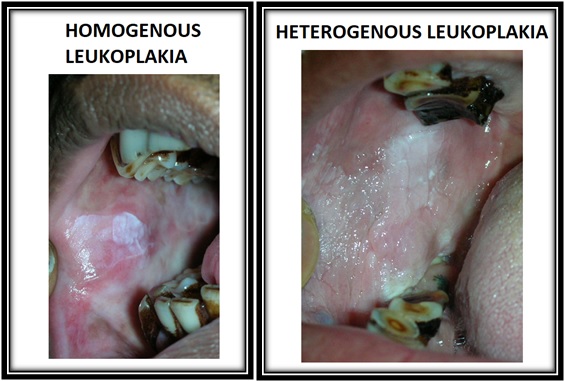
Leukoplakia is defined by the World Health Organization as a white lesion of the oral mucosa that cannot be scraped off and cannot be attributed to another definable lesion (see the first image below). .” It is the most common premalignant lesion of the oral cavity and is clearly associated with tobacco abuse with alcohol acting as an additive factor.
Since leukoplakia often develops without pain or other symptoms, it can go unnoticed until it’s found by your dentist or ENT specialist.
Leukoplakia is broadly classified in to two types
ERYTHROPLAKIA
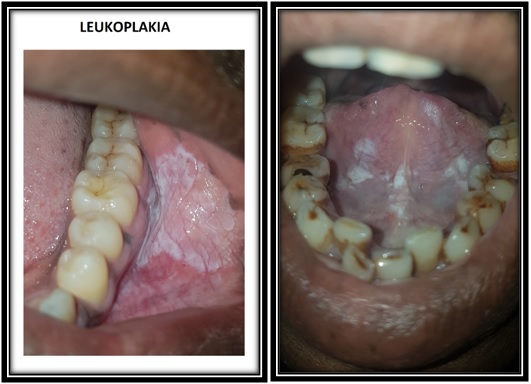
The term erythroplakia is used analogously to leukoplakia to designate lesions of the oral mucosa that present as bright red velvety patch or plaque which cannot be characterized clinically or pathologically as due to any other condition. It is associated with an even higher risk of malignant transformation. Early diagnosis and follow-up is necessary for erythroplakia. At the time of diagnosis, erythroplakia has a high chance of showing signs of precancerous cells. Malignant transformation rates — meaning the chance of precancerous cells turning cancerous — range from 14 to 50 percent.
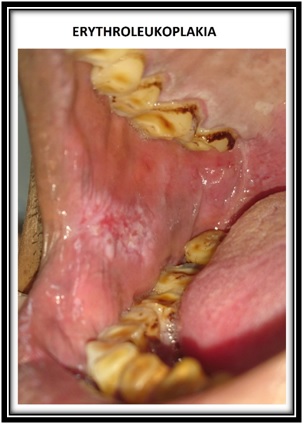
ERYTHROLEUKOPLAKIA
Erythroleukoplakia is a patch with both white and red areas within. Risk of malignancy is same as erythroplakia. Biopsy is always advisable. Surgical excision is recommended irrespective of biopsy findings.
RISK OF MALIGNANT TRANSFORMATION
Presence of moderate to severe dysplasia on biopsy is suggestive of high-risk lesion with a significant risk of malignant transformation. About 5-18% of epithelial dysplasias become malignant.
A greater risk of malignant change in an epithelial dysplasia has been associated with the following factors:
EVALUATION OF ORAL PREMALIGNANT LESIONS
TREATMENT
The gold standard for management of the clinically evident high-grade premalignant disease is surgical excision or laser ablation. However, moderate and low-grade pre-malignancy may be treated with close observation as well.
Various studies have opined that surgical excision of these lesions is better in preventing their malignant transformation, compared to observation and other non-invasive therapies. Laser excision or ablation offers unique advantages over scalpel excision like faster and precise removal of diseased tissue and excellent haemostasis. It has good patient acceptance, low morbidity, and favourable healing.
LASER TREATMENT OF OPLS
The practice of oral surgery has included the use of lasers since the mid-1960s.The CO2 laser has historically been the workhorse in laser surgeries. Use of the laser for management of oral premalignant lesions has got many advantages over other treatment modalities. Complete excision is advisable because it facilitates complete pathologic evaluation and accurate assessment of margins to exclude invasive disease.
Recurrence of leukoplakia and erythroplakia after excisionReported recurrence rates for these lesions are high as 34 %. Whether this relates to continued exposure to risk factors or to the original underlying mechanism that lead to development of primary lesions is unknown. In terms of outcomes , recurrence rate in the same area of excision are around 10 -20 % and cancer in the same area of 3-9 %.